Hi everyone,
Thanks for providing this forum space dedicated to COVID19 work!
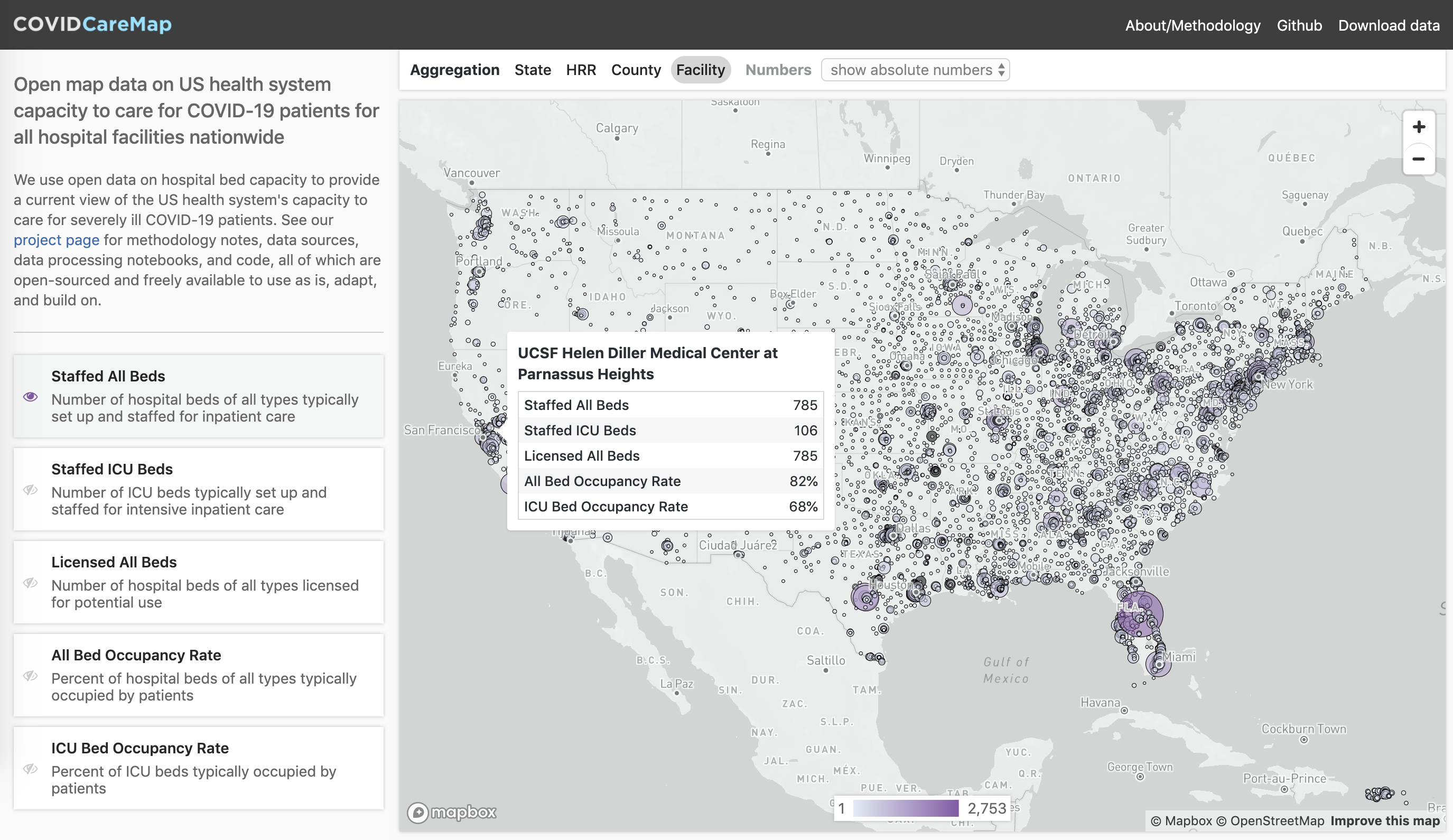
I’ve been.working with a volunteer team of geospatial experts, engineers, data scientists, designers, & communicators to build data, analyses, and tools that help us better understand, anticipate, and act to support and ramp up our local health systems’ capacity (providers, supplies, ventilators, beds, meds) to effectively care for a rapidly growing flow of COVID19 patients.
We’re doing open-source data collection, geospatial analysis, visualizations, and scenario planning tools with a strong focus on the bottleneck of healthcare treatment capacity for critically ill COVID19 patients (i.e. ICU-level beds, equipment, staffing needs). Aiming for high spatiotemporal data resolution (down to individual facility or county level per day across the USA) for current actuals/estimates and scenario projections going forward. It’s USA-centric at the moment but data, tools and knowhow are fully open and intended to be applicable globally.
UPDATED LINKS:
We’re looking for more volunteers and/or collaborations to help us achieve these high-level project goals as quickly and robustly as possible:
-
A. Publish a public dataset that describes the US healthcare system capacity in high spatiotemporal detail.
-
B. Perform an analysis of the healthcare system capacity as compared to disease spread forecasts and publish data about where, when, and how large capacity gaps are anticipated to be.
-
C. Visualize the result of the analysis as well as the disease forecast and healthcare system capacity data in a format that supports healthcare system preparedness and resourcing decisions.
If you’re interested to learn more, start contributing, or collaborate:
- please check out https://github.com/covidcaremap/covid19-healthsystemcapacity,
- join our chat on https://gitter.im/covid19-healthsystemcapacity/community,
- or reply/DM me here
Happy also to answer any questions and share more thoughts and ideas…let me know what you’re thinking!
Thanks, looking forward, and be well,
Dave